I wasn't sure where to go with this today but then I had a situation happen that brought this to the forefront of my mind: breeding.
This is a HUGE issue in my mind. Breeding of animals because they are cute/sweet/the kids want to see puppies or kittens born/my neighbor wants a dog "just like mine" etc are NOT reasons to breed.
Why? Well, first of all, there are millions of cute and sweet dogs and cats in shelters and foster homes all over the USA.
These are some unsettling statistics from the ASCPA
Approximately 5 million to 7 million companion animals
enter animal shelters nationwide every year, and approximately 3 million to 4 million are euthanized (60 percent of dogs and 70 percent of cats).
There are a ton of great stats on this page to really show you the severity of this problem.
What people don't seem to think about is numbers - there are a finite number of homes. If there are 100 homes available that WANT an animal, you breed a litter of 10 and sell to those folks, that represents 10 shelter animals that won't be getting homes. And yes, it IS that simple. People can be educated on where to get pets.
Now, there are some people who want a certain breed of dog or cat. Ok, what about them? Well, there are breed rescues (and no the pets are not all "problem children" or sick animals). There are also search engines like Pet Finder. I know people that have found wonderful pets through them.
If those things aren't getting you what you want, you need to research and find a reputable breeder. By reputable, you want someone who doesn't overbreed, has their animals in a clean and well-socialized environment, who is willing to take an animal back if there is a problem - medical or situational (the really good ones will NOT want their animals to be given away, euthanized etc if they can be fixed/saved), and who, depending on the breed, have done the necessary screening BEFORE breeding to ensure they are not passing down some of the health problems we KNOW can be genetic.
Let me just say this: go with your gut! I've known clients who haven't and have regretted it.
Also consider that ethical breeding serves to improve the breed. Good breeders don't make a huge profit because they are putting money back INTO their dogs with regular vet visits, preventative care and screenings and puppy health checks. AND you must be prepared for the possibility and expense of a C-section. AND it might because the animal has only one puppy (which will probably cost more than the sale of that ONE pup), which sometimes fails to provide enough stimulus for a normal birth. Or because you have a breed that has a high incidence of needing one - Bulldogs, small/toy dogs or mixed breed dogs where the male breed is larger than the female breed.
How about taking your children to the shelter and showing them the importance of being a responsible pet owner? And how people that aren't responsible have created a huge overpopulation problem, particularly with cats. Adopt an animal that needs a home and then have it spayed/neutered if it hasn't already been done.
Snow Leopard

Snow Leopard cub (7 mos old) - Cape May County Zoo
Monday, January 31, 2011
Sunday, January 30, 2011
The Connection Between Animal Abuse and Domestic Violence
And yes there absolutely is one. This has been something that has been known about for years. I'm not a psychologist but it doesn't take much to imagine that someone who can hurt small critters (frogs, birds, etc), drown or burn kittens, tie puppies mouths shut and leave them outside to fend for themselves (yes, these are all REAL things that have happened), would "graduate" to doing bad stuff to kids and adults. Most serial killers started out with insects and animals.
This story prompted me to blog about this:
This story prompted me to blog about this:
Experts: Animal abuse linked to family violence
by Sarah Forgany / KENS 5
Bio | EmailPosted on January 27, 2011 at 10:33 PM
Updated Thursday, Jan 27 at 10:33 PM
SAN ANTONIO -- It's hard to believe an animal could be the target of violence. But experts say along with women and children, cats and dogs often get abused in acts of jealous revenge.
Sallie Scott, President of Friends of Animal Care Services, tells KENS 5 "American Humane Association started a program called link. They saw the link between animal abuse, child abuse, and family violence," Said Scott, "It's very evident in all their studies."
The link Scott adds is in almost 100% of abuse cases and she says animal abuse is becoming more prevalent by the day.
Veterinarians may be the first line of defense for the humans living in an abusive home. The key is spotting animal abuse and then reporting it. The" reporting it" part can be hard. First of all, it's hard to "prove" and secondly, some might fear reprisals from the person doing the abusing.
A good website that discusses this further can be found at:
I've never encountered a case like this myself - where I suspected animal AND human abuse. I have definitely seen animal abuse and the scariest things to me were the two cases where I KNOW a child willfully hurt an animal and didn't seem to care and the parents involved were in total denial. One case involved a cat that was thrown from the top floor balcony inside a house and luckily only sustained some eye trauma that resolved with time and meds BUT it was relatives who brought the cat in and they were fully aware. In fact, they told me of a more serious case involving a cat and this family. I STRONGLY urged them to intervene because of this very link. This child was likely to move on to humans as he grew up.
Saturday, January 29, 2011
How Do You Rehab a Tiger Post-Op?
 |
| A Malayan tiger (subspecies of the Indochinese tiger) in the wild |
A tiger in Germany has become the world's first to be given an artificial hip after a three-hour-operation by a team of veterinarians that she only just survived, Leipzig University said on Thursday.
Girl, as the Malayan tiger at Halle Zoo in eastern Germany is known, had been in visible pain for close to a year because of problems in her right hip joint, the university said.
"Malayan tigers are one of the world's most endangered species, with only around 500 estimated to be living in the wild. This was another reason to operate on Girl," a statement said.
The Rest of the Story is at: http://www.edmontonjournal.com/health/Female+tiger+first+world+artificial/4182858/story.html#ixzz1CQuonClp
For more about these beautiful but critically endangered cats:
Mayalan Tigers
Friday, January 28, 2011
When Stress Can Be Deadly
Those adrenal glands we discussed yesterday can FAIL to produce some of the necessary things that the body needs to function and survive.
There are two main parts of the gland: the cortex (outer layer) and medulla (inner section). They each produce different things. The cortex produces steroids that work on carbohydrate metabolism (corticosteroids) and electrolyte regulation (mineralocorticoids). The medulla produces epinephrine and norepinephrine. This is the "adrenaline" we associate with the "fight or flight" response in animals, including us!
There are two types of deficiencies seen:
1. Both a lack of the corticosteroid and mineralocorticoid production - so no cortisol and the loss of the ability to regulate sodium and potassium (this can REALLY cause some serious problems)
2. A lack of ONLY the corticosteroid portion, so the electrolyte situation is NOT affected.
Some breeds that are more susceptible to this are: Standard Poodles, Portuguese Water Dogs, Great Danes, Rotties, and some terriers but again, any breed can develop this. I have seen it in a number of Labrador Retrievers.
The signs are often vague and can come and go. Then can include vomiting, not eating well, diarrhea, and lethargy. Sometimes they seem to do better after they get some fluids and a shot of a steroid (which can be a general treatment for a LOT of things). They can also have an acute crisis and arrive in a state of collapse. Stresses can cause this to happen - including boarding, grooming, travel, vet visits, etc.
Bloodwork can show some changes that point to this but again, more specific testing is needed to confirm this diagnosis. In this case, we use the ACTH stimulation test. Giving ACTH SHOULD stimulate the adrenal glands to produce cortisol (see yesterday's feedback loop diagram). We also want to measure the ACTH level in some cases to see which of the 2 problems is going on.
The bloodwork can show what first appears to be "kidney failure" and some have misdiagnosed dogs with this when, in fact, they had Addison's. We also want to see what the sodium and potassium levels are. This will be also be checked periodically throughout the animal's life as this requires LIFELONG treatment.
Treatment is a monthly (typically) injection given in the muscle. Owners can be taught to do this at home but I've had clients who were not comfortable with it and would bring their dog in for us to do it. This is a very costly drug - especially since many of the dogs are larger and require a larger dose. Also, they are put on oral prednisone and this may be increased during times of "stress." The dogs that simply have a cortisol deficiency do not need the injection.
There are two main parts of the gland: the cortex (outer layer) and medulla (inner section). They each produce different things. The cortex produces steroids that work on carbohydrate metabolism (corticosteroids) and electrolyte regulation (mineralocorticoids). The medulla produces epinephrine and norepinephrine. This is the "adrenaline" we associate with the "fight or flight" response in animals, including us!
There are two types of deficiencies seen:
1. Both a lack of the corticosteroid and mineralocorticoid production - so no cortisol and the loss of the ability to regulate sodium and potassium (this can REALLY cause some serious problems)
2. A lack of ONLY the corticosteroid portion, so the electrolyte situation is NOT affected.
Some breeds that are more susceptible to this are: Standard Poodles, Portuguese Water Dogs, Great Danes, Rotties, and some terriers but again, any breed can develop this. I have seen it in a number of Labrador Retrievers.
The signs are often vague and can come and go. Then can include vomiting, not eating well, diarrhea, and lethargy. Sometimes they seem to do better after they get some fluids and a shot of a steroid (which can be a general treatment for a LOT of things). They can also have an acute crisis and arrive in a state of collapse. Stresses can cause this to happen - including boarding, grooming, travel, vet visits, etc.
Bloodwork can show some changes that point to this but again, more specific testing is needed to confirm this diagnosis. In this case, we use the ACTH stimulation test. Giving ACTH SHOULD stimulate the adrenal glands to produce cortisol (see yesterday's feedback loop diagram). We also want to measure the ACTH level in some cases to see which of the 2 problems is going on.
The bloodwork can show what first appears to be "kidney failure" and some have misdiagnosed dogs with this when, in fact, they had Addison's. We also want to see what the sodium and potassium levels are. This will be also be checked periodically throughout the animal's life as this requires LIFELONG treatment.
Treatment is a monthly (typically) injection given in the muscle. Owners can be taught to do this at home but I've had clients who were not comfortable with it and would bring their dog in for us to do it. This is a very costly drug - especially since many of the dogs are larger and require a larger dose. Also, they are put on oral prednisone and this may be increased during times of "stress." The dogs that simply have a cortisol deficiency do not need the injection.
Thursday, January 27, 2011
Adrenal Disease: Too Much of a Good Thing
Aka: Hyperadrenocorticism or Cushing's disease.
Adrenal glands are small endocrine glands located just above the kidneys.
They are responsible for an animals response to stress, as well as regulating mineral balance in the body.
The body controls how much of the necessary compounds are released by a very well regulated feed-back system:
So any stressor (this is not just emotional/mental stress but also physical illness which is a "stress" on the body) will stimulate this pathway to direct the adrenal glands to produce and release cortisol.
Cortisol, while having some unhealthy effects, is absolutely essential for any healthy living organism. Yes, you could die if when you were stuck in traffic and freaking out, you did not have a functional pituitary/adrenal axis!
Cushing's disease is on OVERproduction of cortisol. This can be due to a pituitary problem or an adrenal problem. 85-90% is due to pituitary disease. The other 10-15% is caused by an adrenal tumor (50% of these are malignant). We can also CAUSE this (the term "iatrogenic" is used) by giving high/long term doses of steroids. This is why so many vets truly try to avoid this unless there is no other option.
What we first hear from clients is "my dog is drinking and urinating excessively!" In the vet world, this is PU/PD (polyuria/polydypsia). Many times they think it's diabetes. Definitely a possibility. And in fact, we sometimes see dogs that have BOTH diseases.
This can be a sign of other diseases as well, including kidney disease, so of course, blood work and a urine sample are the best way to get a start on figuring this all out.
The signs you see in a Cushinoid dog are the same signs you see if you've ever treated a pet WITH steroids for something: they drink a lot, pee a lot, have a BIG appetite, and often pant and can be restless. Well, this is the same thing only it's coming from an internal source.
Dogs who have Cushings but are also diabetic can be VERY difficult to regulate. Cortisol causes insulin resistance, hence our reason for NOT treating diabetic dogs or cats with any steroids.
Who is at risk for Cushings? poodles, dachsunds, Boston terriers, boxers, beagles..and yes, any breed could get it. Cats can also have this but I personally have never seen or diagnosed this in a cat.
There is a good way to screen dogs: bring a urine sample you collect at home to your vet and they can check for the urine cortisol/creatinine ratio. Since the dog is at home and in a less stressful environment, this can be a great starting point to test. However, keep in mind that you can have a decent number of false positive (so dogs that truly don't have disease are showing a high level). But if they are negative, they likely are truly that.
Many dogs will also have a "pot-bellied" appearance and some loss of hair that is usually symmetrical (even on both sides of dog).
So what do we see that really tells us that your dog has Cushings? Well, the typical abnormality in the bloodwork is an elevated Alkaline Phosphatase, a liver enzyme, that is induced (or increased) in production, when steroids are present. So if your dog is on prednisone or dexamathasone for another issue (skin, orthopedic, etc) this WILL be elevated.
If your dog is NOT on steroids, and is NOT PU/PD, but has a high AlkPhos, it is NOT Cushings and other diagnostics should be pursued (ultrasound, possible liver biopsy, etc).
What we look for is a significant increase over normal (classically 4x the high normal limit).
If we see this, this does not mean your dog absolutely 100% has Cushings. There are other blood tests that will help us truly diagnose this.
Two tests that are used are the Low Dose Dexamathasone Test (LDDT) and the ACTH stimulation test. You can see on the feedback diagram that ACTH SHOULD cause the adrenal gland to produce steroids. In dogs with Cushings, we get a LARGER response than normal. The LDDT is a great test because it allows us to actually determine if your dog's problem is pituitary vs adrenal. Both tests are not invasive and simply involve 1-3 blood draws through the day after we give either ACTH or Dexamathasone as an injection.
If we think it is an adrenal issue, we may recommend an ultrasound to see if there is a tumor of the gland and how invasive it is.
Once we come to this as a diagnosis, there are several medical options to treat this. Untreated disease will progress and carries a very poor prognosis. The treatments include oral drugs, such as Mitotane and Trilostane. Mitotane works by destroying some of the adrenal tissue. Yes, there is a risk of getting rid of too much, so many vets will either make sure you have some prednisone to give or will direct you to give a low dose during treatment or at least, during stressful events (grooming, boarding, etc). Trilostane works by blocking conversion of compounds TO steroids. Once you stop giving it, things revert to normal. This has become the main treatment of choice. Some vets will also use Anipryl (a drug that came out to treat Canine Cognitive Dysfunction aka "doggy Alzheimers"). Studies have shown this drug to be minimally effective. I had one dog that did superb on it. It seems a bit "safer" and was before I had access to Trilostane, which was only approved for us in the US in the past few years.
No matter the treatment, it is not cheap. It can run approx $100/mo to start..and the larger your dog is, the more costly.
Tomorrow we'll discuss what happens when these glands don't produce what they are supposed to!
Adrenal glands are small endocrine glands located just above the kidneys.
They are responsible for an animals response to stress, as well as regulating mineral balance in the body.
The body controls how much of the necessary compounds are released by a very well regulated feed-back system:
So any stressor (this is not just emotional/mental stress but also physical illness which is a "stress" on the body) will stimulate this pathway to direct the adrenal glands to produce and release cortisol.
Cortisol, while having some unhealthy effects, is absolutely essential for any healthy living organism. Yes, you could die if when you were stuck in traffic and freaking out, you did not have a functional pituitary/adrenal axis!
Cushing's disease is on OVERproduction of cortisol. This can be due to a pituitary problem or an adrenal problem. 85-90% is due to pituitary disease. The other 10-15% is caused by an adrenal tumor (50% of these are malignant). We can also CAUSE this (the term "iatrogenic" is used) by giving high/long term doses of steroids. This is why so many vets truly try to avoid this unless there is no other option.
What we first hear from clients is "my dog is drinking and urinating excessively!" In the vet world, this is PU/PD (polyuria/polydypsia). Many times they think it's diabetes. Definitely a possibility. And in fact, we sometimes see dogs that have BOTH diseases.
This can be a sign of other diseases as well, including kidney disease, so of course, blood work and a urine sample are the best way to get a start on figuring this all out.
The signs you see in a Cushinoid dog are the same signs you see if you've ever treated a pet WITH steroids for something: they drink a lot, pee a lot, have a BIG appetite, and often pant and can be restless. Well, this is the same thing only it's coming from an internal source.
Dogs who have Cushings but are also diabetic can be VERY difficult to regulate. Cortisol causes insulin resistance, hence our reason for NOT treating diabetic dogs or cats with any steroids.
Who is at risk for Cushings? poodles, dachsunds, Boston terriers, boxers, beagles..and yes, any breed could get it. Cats can also have this but I personally have never seen or diagnosed this in a cat.
There is a good way to screen dogs: bring a urine sample you collect at home to your vet and they can check for the urine cortisol/creatinine ratio. Since the dog is at home and in a less stressful environment, this can be a great starting point to test. However, keep in mind that you can have a decent number of false positive (so dogs that truly don't have disease are showing a high level). But if they are negative, they likely are truly that.
Many dogs will also have a "pot-bellied" appearance and some loss of hair that is usually symmetrical (even on both sides of dog).
So what do we see that really tells us that your dog has Cushings? Well, the typical abnormality in the bloodwork is an elevated Alkaline Phosphatase, a liver enzyme, that is induced (or increased) in production, when steroids are present. So if your dog is on prednisone or dexamathasone for another issue (skin, orthopedic, etc) this WILL be elevated.
If your dog is NOT on steroids, and is NOT PU/PD, but has a high AlkPhos, it is NOT Cushings and other diagnostics should be pursued (ultrasound, possible liver biopsy, etc).
What we look for is a significant increase over normal (classically 4x the high normal limit).
If we see this, this does not mean your dog absolutely 100% has Cushings. There are other blood tests that will help us truly diagnose this.
Two tests that are used are the Low Dose Dexamathasone Test (LDDT) and the ACTH stimulation test. You can see on the feedback diagram that ACTH SHOULD cause the adrenal gland to produce steroids. In dogs with Cushings, we get a LARGER response than normal. The LDDT is a great test because it allows us to actually determine if your dog's problem is pituitary vs adrenal. Both tests are not invasive and simply involve 1-3 blood draws through the day after we give either ACTH or Dexamathasone as an injection.
If we think it is an adrenal issue, we may recommend an ultrasound to see if there is a tumor of the gland and how invasive it is.
Once we come to this as a diagnosis, there are several medical options to treat this. Untreated disease will progress and carries a very poor prognosis. The treatments include oral drugs, such as Mitotane and Trilostane. Mitotane works by destroying some of the adrenal tissue. Yes, there is a risk of getting rid of too much, so many vets will either make sure you have some prednisone to give or will direct you to give a low dose during treatment or at least, during stressful events (grooming, boarding, etc). Trilostane works by blocking conversion of compounds TO steroids. Once you stop giving it, things revert to normal. This has become the main treatment of choice. Some vets will also use Anipryl (a drug that came out to treat Canine Cognitive Dysfunction aka "doggy Alzheimers"). Studies have shown this drug to be minimally effective. I had one dog that did superb on it. It seems a bit "safer" and was before I had access to Trilostane, which was only approved for us in the US in the past few years.
No matter the treatment, it is not cheap. It can run approx $100/mo to start..and the larger your dog is, the more costly.
Tomorrow we'll discuss what happens when these glands don't produce what they are supposed to!
Wednesday, January 26, 2011
Diabetes Mellitus
This is one of the most common endocrine disorders we see in our pet population. In pets, it is due to a lack of insulin production by the pancreas or a poor response to the insulin they are producing. Therefore, our pets are usually insulin dependent and generally require for us to supplement them via insulin injections. The cells in their body cannot process sugar so they “think” they are starving, which is why our diabetic pets tend to have a great appetite but lose weight.
For both dogs and cats, obesity is a risk factor. There ARE certain breeds of dogs that have a higher risk: Keeshonds, miniature pinchers, Cairn terriers, poodles, dachsunds, mini schnauzers and beagles. But this is possible IN any breed or mixed breed dog.
This is generally a problem of older pets (>8yrs of age) though I have absolutely seen it in younger cats and dogs (I can think of several 5 and 6 yr old pets off the top of my head).
Risk factors that may predispose your pet to this: being overweight and pancreatitis (inflammation of the pancreas). Pancreatitis will be covered another day but tends to occur more chronically (and often under the radar) in cats. Some drugs, like steroids (prednisone, Depo-Medrol injections, dexamethasone) can predispose a pet to DM.
The primary complaint from the pet owner is that the animal is drinking excessively and urinating excessively, sometimes having accidents in the house/out of the litterbox. There is also usually some weight loss especially as this goes on longer.
It is easy to test for - in routine bloodwork and a urinalysis. In cats, stress can cause their blood sugar (glucose) level to be high. Stressed cats can have a blood glucose of up to 300 mg/dl and NOT be diabetic. If we see it above that, we look at the urine and the clinical signs the pet is showing.
If there is still any uncertainty, we can have the lab run a fructosamine level on the blood. THIS tests for a protein bound portion that is absolutely NOT affected by stress or any one point in time. In fact, it allows us too “view” the past few weeks of a pet’s blood sugar levels as a general average value. We often use it as a monitoring tool once the pet is on insulin.
Initially, if we find your pet to be diabetic, we will prescribe insulin injections (most often twice a day) and some dietary changes. This is key in cats as they can often AVOID or come off of injections by being put on a high protein diet (sometimes referred to as “CATkins”). There have been cats that have “revereted” to NON diabetic states once they are eating more of a canned food diet.
Dry foods are great...for pet owners. They are cheaper and keep for a longer period of time. However, they often have a higher amount of carbohydrates in them, which can be a problem for the feline gastrointestinsal system, which is designed for an obligate carnivore (meat eater!).
As far as insulin types, I won’t go into great depth on this. Why? Well, over the years I’ve been in practice, the insulin available to us as veterinarians changes often. And trust me when I say that working with diabetic pets is truly ART as much as science.
For dogs, most commonly, we have used NPH, which is a HUMAN recombinent insulin. There have been veterinary formulations, which have come on and off the market. The cats have done the best with PZI (porcine zinc insulin) but 1)this can be difficult to get at times 2) you need to have a reliable source that is consistent in what it is producing. Glargine, a human insulin, has also been used with success in cats, but it is costly. Still, some have found that by starting with glargine and a diet change to a protein based diet, in a few months, they only need the diet.
Initially, some vets may want to keep your pet in the hospital to see how they do with a given dose of insulin. They will take measurements approximiately every 2 hours. We refer to this as a glucose curve. Not all vets will do this. Some prefer NOT to do it with cats.
There are some things that can make a diabetic pet difficult to regulate: any sources of infection (including dental disease), being unspayed, other diseases, like Cushing's (tomorrow's topic) and medications (steroids like prednisone). These need to be dealt with to help your pet do well.
In dogs more than cats, unregulated diabetes often leads to cataracts. Unregulated animals will also continue to lose weight. We do not tend to see the other problems (like kidney issues and circulatory problems with the feet, etc) that are seen in human diabetic patients. Unregulated or untreated pets can end up in a severely depressed and comatose-like state (known as diabetic ketoacidosis) that requires hospitalization and intensive care with IV fluids and doses of regular insulin to get the blood sugar down.
It is very easy to teach a pet owner how to give an insulin injection. The needle size we use is smaller than a vaccine needle. There are different syringes depending on insulin type so do NOT think they are interchangeable. There are U-40 and U-100 insulins out there.
One quick note about oral hypoglycemics that people use. In my experience, these do not work very well. They can work for a few so it could be worth trying especially in a cat that may be difficult to give a shot to but I've found even in those cases, eventually, it no longer works.
Your vet and their staff will go over all the details of caring for a diabetic pet. It may seem overwhelming at first, but trust me, many pets owners deal with this quite successfully. Every pet is different in how they respond.
Your vet and their staff will go over all the details of caring for a diabetic pet. It may seem overwhelming at first, but trust me, many pets owners deal with this quite successfully. Every pet is different in how they respond.
Yes, you can test at home, especially if you feel comfortable with a little skin prick in the cat or dog’s ear or foot pad. Ask your vet about which monitor to use. There are a few that have been made specifically for animals.
But do not change doseages without consulting with your vet. Trends are what is important. There can be a tendency to try to too closely tighten where the blood sugar level is and this can cause problems of its own.
I advise owners to watch the drinking/urinating. This should go down and back to what was considered normal as the pet gets better regulated. Regular rechecks of bloodwork AND weight checks will help us know if the pet is regulated.
Frequent communication between you and your vet are key to keeping your pet healthy during this time.
Some key points I REALLY want you to take home:
- Never ignore changes in your pet’s habits
- If your animal is diabetic, do NOT give insulin if the pet is NOT eating and please CALL your vet
- Watch for signs of low blood sugar (wobbliness, seizures) and keep some Karo syrup around for rubbing on the gums, lips, etc. CALL YOUR VET!
- If your schedule gets thrown off by a few hours, do not give insulin, it’s better for a pet’s sugar to be too high for a short time then to dip too low
- If you are giving insulin and the pet moves and you aren't sure how much they got, don't try to figure it out. You could give too much. Just do the next dose as usual.
- Keeping weight OFF your pet is easier than getting it off so start young! This may prevent diabetes all together.
Tuesday, January 25, 2011
Thyroid Disease in Cats: HYPERthyroidism
Unlike dogs, cats have thyroid glands that become overactive. This is one of the top three diseases we see in older cats (generally those >7yrs old). The other two are diabetes mellitus and kidney disease.
The signs for all three of these diseases can be similar, so a baseline blood panel and urinalysis are the best way for your vet to sort it out. Don’t forget, they can have more than one thing going on at a time too, which may change the way we handle the treatment and follow-up care of your cat.
Signs include but are not limited to: weight loss despite a generally great (sometimes RAVENOUS) appetite, increased drinking/urination, hyperactivity, and behavioral changes (including aggression, vocalizations without cause, not using the litterbox). There are a very small percentage (5%) of cats that go the opposite way though. These cats become lethargic and don’t eat well.
 |
| Skinny cat with unkempt coat that is often seen in cats with thyroid disease. |
In most of these cases, on a physical exam of the cat we find the thryoid glands to be enlarged (in a normal cat, these are not normally something we can feel). Many times the cat also has a rapid heart rate (tachycardia).
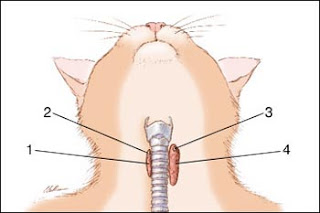 |
| 1. normal thyroid gland 2. and 3. parathyroid glands 4. enlarged thyroid gland |
The T4 IS generally a great way to determine if your cat has a thyroid problem. If this is normal but your vet really suspects hyperthyroidism, they may want to add the Free T4.
There are several treatments. The most common is to give a twice a day medication called methimazole. We can have a liquid compounded and flavored for your cat or you can give pills. This is a lifelong treatment. This drug works by blocking excess production of thyroid hormone and doesn't destroy any tissue, which is why it needs to be given regularly.
There are also trans-dermal formulations (goes through the skin). These do seem to work fairly well. They are also compounded for us by special pharmacies and are rubbed on the ears. This is sometimes used when a cat can't tolerate any oral formulations.
As with any animal on chronic medication, we will want to do a follow blood panel (checking those kidney values AND the thyroid level). After the cat's thyroid is in the normal range, rechecks can be done every 6 months to a year.
The other primary way to deal with it is to have your cat treated with I131(radioactive iodine). This is a one time treatment! Don’t worry, this is safe. It IS done at only certain facilities and your cat will stay a few short days. This is NOT done initially because sometimes cats that have hyperthyroidism have “hidden” kidney disease. The higher metabolism that hyperthyroidism produces results in more blood flow through the kidneys. When we correct this, sometimes we unmask this other disease process. So we always start with the first option - then we can back down if we need to.
This is a great way to go if your cat is younger when diagnosed and/or you have difficulty medicating twice a day for the remainder of the cat’s life. It is initially more expensive up front but if your cat is 10 when diagnosed and lives until she’s 20, it will be cheaper in the long run.
A good website that discusses this is: Radiocat. They do not have any locations in this part of PA or anywhere in NJ. For those living in the Lehigh Valley, there are places that do offer this: Valley Central Nuclear Medicine, Metropolitan Veterinary Associates and The University of Penn School of Veterinary Medicine.
I did not discuss surgery which has been used in the past to treat this disease, because it has generally fallen out of favor, especially since we have other great options.
If you cat shows ANY changes in her normal behaviors, no matter how subtle, please make an appointment with your veterinarian.
Monday, January 24, 2011
Thyroid Disease in Dogs: HYPOthyroidism
A good friend asked me to expound on this topic.
It’s a good one too because it can be a bit of a murky diagnosis. There are many things that need to be taken into account and it's NOT based simply on a blood test.
Most pet owners would love for their dog to have a thyroid issue. Why? Because, unfortunately, the majority of pets are overweight.
A low thyroid is GENERALLY not the reason however. Remember, our pets don’t make their own meals, buy or give their own treats or open the refrigerator door and find a midnight snack (for the MOST part !).
It takes a good 80-90% of the gland to be destroyed to see TRUE dysfunction.
What do we see in dogs with TRUE thyroid dysfunction?
Most of the signs are generally dermatologic (skin) and a decreased metabolic rate (weight gain, lethargy, etc). There are some less common signs that include neurologic diseases (seizures, etc).
What blood test do we use?
A good baseline is the T4 level. However, this is more of a screening tool. There are a lot of other things that can cause this level to be low, even though the dog’s thyroid gland is functioning perfectly normally. We must take this number as part of the BIG PICTURE - what is going on with this dog? - other illnesses? is the dog truly showing any signs of hypothyroidism?, is the animal on any medications that might cause this to be lower than normal (phenobarbital, certain antibiotics in the sulfa class, steroids) ?
A dog that has an illness that is suppressing it’s thyroid level is termed “euthyroid (normal thyroid) sick syndrome.” Once that issue is dealt with and the dog is fine, we can recheck the thyroid level. Experts think this is some sort of protective mechanism for the dog. If they are ill with some disease process, their metabolism slowing down may help NOT drain their resources as quickly.
If we do indeed STILL suspect hypothyroidisim, we will want to run a few further tests including a FREE T4 and maybe a TSH (thyroid stimulating hormone level).
The Free T4 measure what most people think of as the “active” form of the thyroid molecule. But we must remember that this molecule can also be affected by other illnesses going on in the dog too.
What if the dog IS hypothyroid?
Then we need to start on a thyorid hormone supplement available through your veterinarian. This is not an expensive drug but it is LIFELONG. Most vets will want a recheck of that T4 or FreeT4 level in 1-2 months, usually at 4-6 hours post pill (this is when peak blood levels are reached). We can adjust the dosage from there - based on the level and how the dog is doing.
What if it's NOT hypothyroid?
...and your dog is still gaining weight ? (then very likely he is being overfed - remember if he is eating 2 pieces of kibble a day and is gaining weight, he's NOT burning those calories off) ...so back it down, limit treats, and increase exercise or...you may end up needing more info on Wednesday's topic - diabetes.
... and your dog has skin issues? Well, that could and will likely be a whole week or more in itself.
Subscribe to:
Comments (Atom)











